Plantar fasciitis is the most common cause of heel pain (also called hedonistic). It occurs mainly among athletes (but can also affect sedentary people who do not play sports) and is caused by the continuous repetition of excessive overloads at the breech level, on the plantar fascia. It’s a relatively frequent pathology. It represents, in fact, about 10% of all pathologies affecting the foot and is one of the most common causes of heel pain. The subjects most affected by the problem are those who practice sports such as running, basketball, football, volleyball, long jump, etc., but also those suffering from obesity and diabetes.
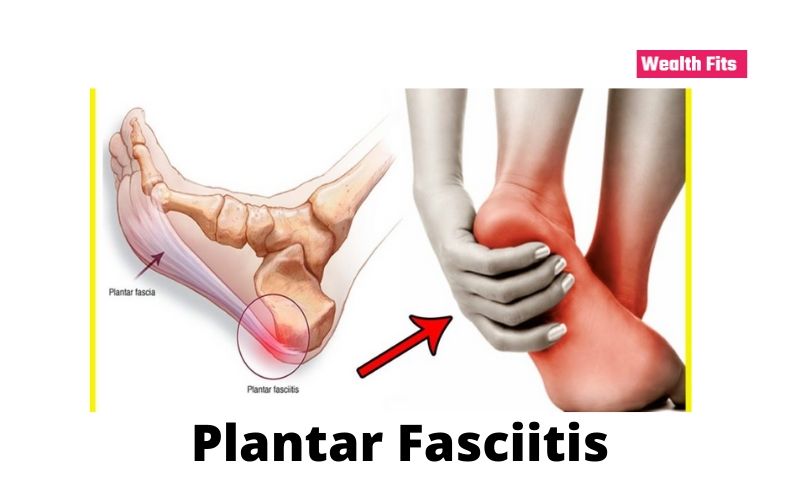
Before delving deeper into the problem of plantar fasciitis, it is worth analyzing the affected district anatomically.
Plantar fascia (or plantar Aponeurosis)
The plantar fasciitis is the ‘ inflammation of the plantar fascia, a band of elastic tissue that extends from the heel to the metatarsal area, located in front of the fingers. This structure has an essential role in walking because it is one of the main responsible for maintaining the plantar arch, and serves to absorb and return the energy produced when the foot hits the ground. In addition, it is responsible for protecting the metatarsal by avoiding excessive flexion of the fingers.
In this pathology, the bones of the foot (heel, metatarsal, and phalanges) and the muscle structures of the foot, which are stressed, should be taken into consideration.
By touching the foot, we can quickly feel the plantar fascia is a fibrous, and less elastic, fabric located in the inner part of the foot, which is plantar fasciitis tends to become very hard and painful even out of load.
Causes and risk factors of plantar fasciitis
As we age, the plantar fascia loses elasticity and can no longer stretch well. The fat pad on the heel thins and cannot absorb the shocks that arise when walking. Excessive stress on the heel causes inflammation in the insertion of the bundles or, worse, along with their entire extension.
Plantar fasciitis can arise due to countless factors, often combined with each other.
Risk factors for plantar fasciitis:
- Age: Plantar fasciitis affects active patients between the ages of 40 and 70. It is one of the most frequent orthopedic ailments related to the foot.
- Anatomy: Some anatomical features, such as flat feet or hollow feet, can also lead to episodes of fasciitis.
- Diabetes
- Obesity
- Sports and work activities: Activities that stress the heel and adjacent tissues a lot, such as endurance running, dancing, or aerobics, can contribute to the early onset of plantar fasciitis.
- Inadequate footwear: Shoes too wide, with excessively thin soles or with too high heels, etc.
What are the symptoms of plantar fasciitis?
In the case of plantar fasciitis, subjects affected by this pathology report acute pain in the center of the heel, which in some cases can radiate under the sole of the foot or around the edge of the same heel as a band. In the morning, as soon as you get out of bed and take your first steps.
-
Getting up after sitting for a long time
-
At the end of a very intense sport (running, football, etc.)
-
At the end of the day, after standing for many hours.
Even the course of symptoms can be very different from person to person; in less severe cases, it is a non-acute pain that persists throughout the duration of sporting activities or daily activities, but which, being not very intense, still allows walking, running or jumping. The onset of symptoms may also be different: it may appear in an acute form or be progressive.
The classic pain in the morning is caused by the tension of the plantar fascia and Achilles tendon, which during the night, shortens with the foot in the rest position, and as soon as you get off the bed, with your foot at 90 °. They cannot extend, causing pain under the heel.
What to do?
First of all, give yourself a timing. If the ailment lasts more than 10/15 days, it is good to have your foot examined. Your family doctor should be able to give you the first indications. Cryotherapy (applications of local ice or immersion of the foot in ice water) ) for 15 ‘, use “running” type shoes with rear support (avoid “ballerinas” or “all-star” type shoes). Rest from active sports activities (i.e., running or otherwise standing), application of local anti-inflammatory agents. This is the ABC of remedies for symptoms.
If it doesn’t pass?
You need to do an in-depth study. Contact an orthopedic specialist in the foot. He will visit you and can ask you for in-depth diagnostic analyzes (usual slab in charge and ultrasound). Do not go it yourself, believing that an MRI is always the best way to get a diagnosis. Otherwise, the radiologist will not have “focus” to be explored.
How to make Plantar Fasciitis Diagnosis
Plantar fasciitis is usually diagnosed after a careful clinical evaluation of the case. They are taking into consideration the various risk factors that we have listed above. The prescription of diagnostic tests. Such as x-rays, CT scans, or magnetic resonances is not essential in the diagnosis phase. But it is useful to rule out further causes of heel pain (such as fractures, arthrosis, tumors, etc.).
The main examination is certainly the Rx plate. Both to exclude the heel spur and to highlight the integrity of the structures. The doctor can integrate the diagnosis with the ultrasound to evaluate the quality of the tissues—possibly the resonance (even if the cost-benefit does not recommend its use).
Certainly, as for any other pathology, the diagnosis of fasciitis is more complete if it is the result of the synthesis between clinical examination and instrumental examinations.
How is Plantar Fasciitis Treated?
The purpose of the treatments that are carried out for plantar fasciitis is to reduce inflammation. Eliminate painful symptoms, recover the elasticity of the structures affected (plantar aponeurosis, Achilles tendon), in order to improve general posture and plantar support.
The cure for plantar fasciitis must be divided into two phases, which must be absolutely consequential. The second aims to eliminate the root problem to avoid recurrence and hit the underlying problem.
In the first phase, we can list various types of treatment, to be carried out simultaneously:
- REST: very often underestimated by patients, rest is a fundamental component in the recovery process. It is an integral part of rehabilitation and is the first thing to do when you notice the symptoms of plantar fasciitis. Stop training for a few weeks and avoid walking or standing too long, especially on hard surfaces. Initial rest usually helps relieve pain and reduce inflammation.
- Use of suitable shoes: sometimes incorrect footwear can act as a starter to the disease, and prolonged use of incorrect footwear leads to the chronicity of the problem, in addition to the frustration of the treatments. There are specific insoles for plantar fasciitis that can help redistribute pressure and reduce strain on plantar fasciitis.
- CRYOTHERAPY / ICE: ice is a very useful and easily available remedy, especially in the early stages of treatment, when the patient experiences acute pain, as it alleviates local symptoms. It is advisable to apply an ice pack under the heel or, in any case, the plantar fascia several times a day for about 20 minutes each time. This situation massages and helps to reduce plantar fasciitis a lot.
STRETCHING EXERCISES
- Since plantar fasciitis is connected to a strong retraction and rigidity of the soft tissues present in the plantar and posterior area of the foot (plantar fascia-Achilles tendon), stretching these structures is fundamental in recovering elasticity of the same by eliminating one of the triggers.
- ANTI-INFLAMMATORY DRUGS: taking anti-inflammatory drugs is useful for decreasing inflammation. According to our experience, oral (granular / tablets, etc …) or topical (creams/gel) administration does not always have decisive effects. INFILTRATION: As we said earlier, when oral or topical drugs have no effect. It is useful to resort to local cortisone infiltrations. Always after a medical examination, which will accompany the rehabilitation and help the work.
- PLANTARIES AND TALLONIERE: The application of these orthoses inside the shoes often help the solution of the problem by unloading the areas most subjected to pressure.
How to Get Water Out of Your Ears
What is the physiotherapy treatment to treat plantar fasciitis?
Physiotherapy represents the Election treatment for the treatment of plantar fasciitis: unfortunately, it must be done well, remembering not to miss any steps and rely on valid professionals.
THE tecarterapia then provides a great help in reducing inflammation. Edema and stimulate tissue to regenerate. Another always very valid treatment is the high energy laser. Which greatly promotes healing. To these treatments on the symptom. So rebalancing posture is the best solution with Mezieres postural re-education.
Therapies? Plantar? Or what else?
Here too, it is good to do some clarity. I state that I bring you my experience. Obviously, it is not law. It is based on collaborations with orthopedists specialized in this anatomical trait and observations on hundreds of patients (sports and non-sports) treated in about ten years.
First of all, it is good to take care of the foot, which is to overcome inflammation. From the point of view of instrumental therapies, you can very well bypass the classic analgesic therapies. Those that only aim to make you feel less pain.
It is good to go towards the so-called ” biostimulation therapies “That is able to accelerate the natural repair and healing processes of our body”: ecotherapy (not surrogates), laser therapy (medium or high power), resonate, pronexibus … up to the focused shock waves (ESWT) as the “last beach “or suitable for sportsmen with little time available to return to the pitch. It is good to know that the tendon, by its nature, has decidedly slow healing times, also due to its poor blood supply. Who promises you miracles in a session or something like that … maybe he doesn’t know physiology well! Therapies are usually accompanied with plantar fascia stretching exercises,
Focused Shockwaves (ESWT)
They are undoubtedly the approach that has the best numbers from the healing point of view. About 80% of my cases have solved the problem.15% partially, 5% not (data from Equipe www.equipe.ro. it ). FALSE! Others say that they are so painful that it is better to avoid them … FALSE! They have a defect, yes, they are expensive. They need four sessions (maximum 6 in very serious cases) … if they offer them at bargain prices, be careful, often they are waves of RADIALS collision … another thing!
Why do I have a plantar fasciitis doctor?
At this point, it is good to ask yourself a question: but why does this plantar fasciitis come?
Almost always, there are several concomitant factors: shoes that are not suitable for the activity carried out or habits. Overweight and postural disorders, not forgetting that posture is not like faith.
So if you are lucky enough to be able to compare yourself with a posturologist physiotherapist, he will be able to evaluate and check if fasciitis has left aftermath and ascending disorders (i.e., on joints above the feet: knee, hip, etc.). As often happens, it is really your foot that needs to change support.
Hence the ” baropodometric ” analysis will be able to establish how the loads (i.e., your body weight) are distributed on the feet if you do this examination in the midst of your pains. That is, in the beginning … do you think it will be reliable? Or will it give the image of a foot that “runs away” from pain? Consequently, the proposed correction would also be fictitious … right?
What to do with a pimple in ear